AUA NEWS
JUNE 2023

The New York Section AUA EMPIRE Collaborative:
Hands-on Urology Intern Boot Camp
Gina M. Badalato, MD
Columbia University Irving Medical Center, New York
Alexander Small, MD
Montefiore Medical Center, Bronx, New York
Christopher B. Anderson, MD, MPH
Columbia University Irving Medical Center, New York
Both senior medical students and residency training programs have an interest in adequately preparing students to begin intern year. Successful models of pre-internship preparatory courses have been embedded into some medical school curricula and involve high yield clinical information and skills-based learning.1-3 Surgical residency programs in particular have employed these training sessions as part of new resident orientation, often utilizing virtual, didactic, and simulation-based components in their course designs.4-7 With the incorporation of intern year into urology graduate medical education programs in 2019, urology programs may now be required to provide intern preparation that had traditionally been offered by general surgery departments.8
In 2019, Tabakin and colleagues piloted the feasibility of a multi-institutional urology boot camp for incoming residents.9 The program involved 11 junior urology residents at 4 New Jersey residencies. The seminar included lectures and practical sessions on urethral catheterization and dilation, suprapubic tube insertion, and initiation of bladder irrigation. Following the course, 91% felt better prepared to start their intern year, and the authors demonstrated a durable impact on participants at 6-month followup.
The New York Section (NYS) of the AUA Educational Multi-Institutional Program for Instructing REsidents (EM PIRE) collaborative sought to implement a similar pilot program to meet the needs of incoming urology residents in the New York area. As many senior medical students had their clinical years disrupted by COVID, offering a course that was both live, hands on, and predominantly skills focused was an important concept in the development of this curriculum. With the support of the NYS AUA, this group moved outside of the virtual classroom to design a training program that focused on practical skills for incoming interns and junior residents.
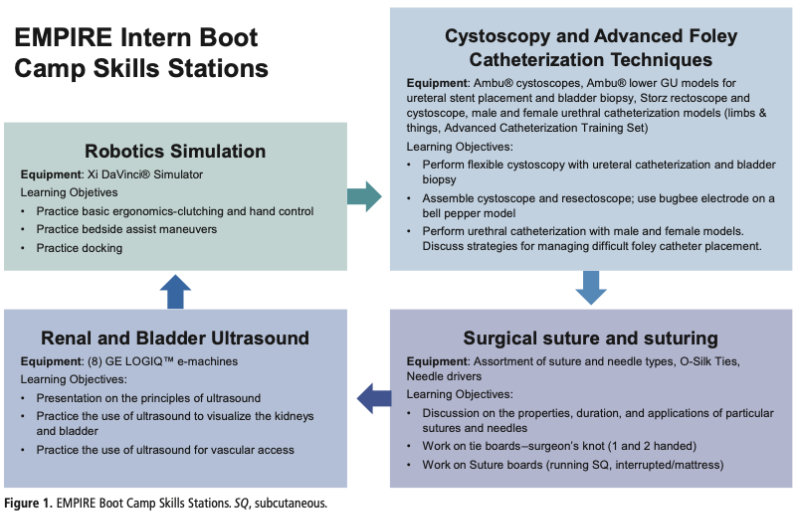
On June 10, 2022, the inaugural EMPIRE Intern Boot Camp was held at the Mary & Michael Jaharis Simulation Center at Columbia University Vagelos College of Physicians and Surgeons in Manhattan. The course was organized into 4 skills stations, including robotics simulation, ultrasound skills, cystoscopy and advanced Foley catheterization techniques, and surgical suturing (Fig. 1). A moderated panel of practical tips from current interns was held over lunch, followed by an interactive lecture on urological emergencies. Twenty-nine junior residents, 4 senior resident preceptors, and 14 faculty from 10 institutions in the NYS AUA participated in the EMPIRE Intern Boot Camp (Fig. 2). Among the participants, 5 trainees were rising postgraduate year 2 residents and the remainder were incoming interns. Following completion of the course, 11 faculty (78%) and 23 trainees (79%) completed the post-course survey.
The resident survey evaluated the effectiveness of each skills station, the lecture, and the overall impact of the course. On a 5-point Likert scale, with a higher number being more favorable, mean scores for each of the skills stations were high: 4.39±0.64 for the renal-bladder ultrasound, 4.52 ± 0.77 for suturing and knot tying, 4.74±0 0.61 for the fundamentals of robotic surgery, 4.78±0.51 for introductory cystoscopy, and 4.83±0.38 for urethral catheterization. Over 90% of junior residents (21/23) strongly agreed the course provided a high-yield overview of urological emergencies. Participants were also questioned about the general impact of the course. Among respondents, 87% strongly agreed the course was effective for meeting and networking with residents at different programs. The same percentage of residents strongly agreed the course 1) was fun and engaging, and 2) made them feel better overall prepared for their upcoming residency rotations.
The faculty also completed a post-course survey. When questioned about skills sessions for interns at their institutions in prior years, 5 faculty noted no prior advanced skills sessions were offered, while 5 stated sessions were offered through their own department and 1 reported similar training was provided through their department of surgery. Among those 6 faculty endorsing prior training workshops for their interns, all 6 incorporated surgical suturing, 4 included an introduction to robotics and laparoscopy, and 4 featured cystoscopy. Nearly all (10/11) faculty responded that this course should continue in future years.
This pilot demonstrates the feasibility and effectiveness of a multi-institutional hands-on seminar for skills and high-yield knowledge acquisition among junior urology trainees. Overall, the session was highly rated by both the residents and faculty, serving as both a valuable educational experience as well as an important sectional networking and community-building activity. As formal programs to address the skills-based training requirements for junior urology residents continue to grow, a collaborative approach, both among institutions and educators, may help to best fulfill this need.

- Varma B, Mirson L, Vanderberg R, Donovan AK. A survey of internal medicineinternsregard- ing themost useful topicsto includein an internal medicine track of a “get ready for residency boot camp” course. Med Sci Educ. 2021;31(1):37-40.
- Neylan CJ, Nelson EF, Dumon KR, et al. Medi- cal school surgical boot camps: a systematic re- view. JSurgEduc. 2017;74(3):384-389.
- Zhang J, Zilundu PLM , Zhang W, et al. The use of a surgical boot camp combining anatomical education and surgical simulation for internship preparedness among senior medical students. BMC Med Educ. 2022;22(1):459.
- Kassam AF, Singer KE, Winer LK, et al. Ac- quisition and retention of surgical skills taught during intern surgical boot camp. Am J Surg. 2021;221(5):987-992.
- Bondzi-Simpson A, Lindo CJ, Hoy M , Lui JT. The otolaryngology boot camp: a scoping re- view evaluating commonalities and appraisal for curriculum design and delivery. JOtolaryngol Head Neck Surg. 2022;51(1):23.
- Young M , Lewis C, Kailavasan M , et al. A sys- tematic review of methodological principlesand delivery of surgical simulation bootcamps. Am J Surg. 2022, 223(6):1079-1087.
- Bhashyam AR, Dyer GSM. “Virtual” boot camp: orthopaedic intern education in the time of COV ID-19 and beyond. J Am Acad Orthop Surg. 2020;28(17):e735-e743.
- American Board of Urology.General requirements. https://www.abu.org/residency-requirements/.
- Tabakin AL, Dave PJ, Srivastava A, Polotti CF, Sterling JA, Elsamra SE. The feasibility and efficacy of a multi-institutional urology boot camp for incoming urology residents. Urology 2021;153:69-74.
Source: